Posted on 10/18/2021 7:48:32 AM PDT by Red Badger
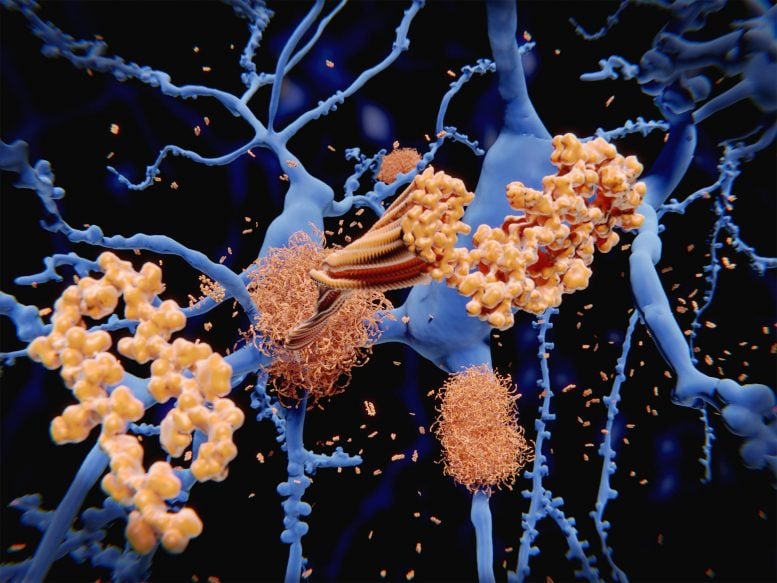
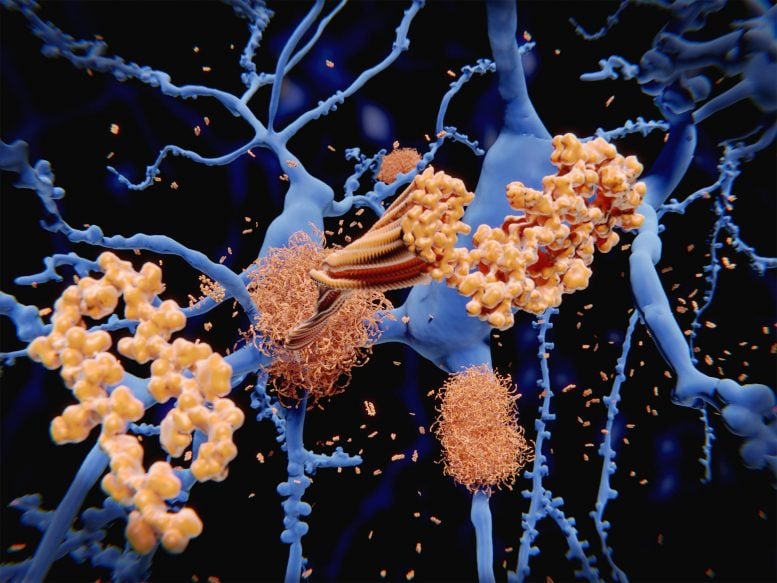
Amyloid protein (orange) forms clumps among neurons (blue). Amyloid in the brain is one of the proteins associated with Alzheimer’s disease.
================================================================================
In a major breakthrough, researchers at Massachusetts General Hospital (MGH) have discovered how amyloid beta — the neurotoxin believed to be at the root of Alzheimer’s disease (AD) — forms in axons and related structures that connect neurons in the brain, where it causes the most damage. Their findings, published in Cell Reports, could serve as a guidepost for developing new therapies to prevent the onset of this devastating neurological disease.
Among his many contributions to research on AD, Rudolph Tanzi, PhD, vice chair of Neurology and co-director of the McCance Center for Brain Health at MGH, led a team in 1986 that discovered the first Alzheimer’s disease gene, known as APP, which provides instructions for making amyloid protein precursor (APP). When this protein is cut (or cleaved) by enzymes — first, beta secretase, followed by gamma secretase — the byproduct is amyloid beta (sometimes shortened to Abeta). Large deposits of amyloid beta are believed to cause neurological destruction that results in AD. Amyloid beta formed in the brain’s axons and nerve endings causes the worst damage in AD by impairing communication between nerve cells (or neurons) in the brain. Researchers around the world have worked intensely to find ways to block the formation of amyloid beta by preventing cleavage by beta secretase and gamma secretase. However, these approaches have been hampered by safety issues.
Despite years of research, a major mystery has remained. “We knew that Abeta is made in the axons of the brain’s nerve cells, but we didn’t know how,” says Tanzi. He and his colleagues probed the question by studying the brains of mice, as well as with a research tool known as Alzheimer’s in a dish, a three-dimensional cell culture model of the disease created in 2014 by Tanzi and a colleague, Doo Yeon Kim, PhD. Earlier, in 2013, several other MGH researchers, including neurobiologist Dora Kovacs, PhD (who is married to Tanzi), and Raja Bhattacharyya, PhD, a member of Tanzi’s lab, showed that a form of APP that has undergone a process called palmitoylation (palAPP) gives rise to amyloid beta. That study indicated that, within the neuron, palAPP is transported in a fatty vesicle (or sac) known as a lipid raft. But there are many forms of lipid rafts. “So the question was, Which lipid rafts? And which ones are most relevant to the neuronal processes making up the neural networks of the brain?” says Tanzi.
The new investigation revealed that palAPP is stabilized and prepared for cleavage by beta secretase in special lipid rafts within the neuron known as mitochondria-associated endoplasmic reticulum membranes (MAMs). “We showed for the first time not only that the MAM is where palAPP is processed by beta secretase to make Abeta, but that this happens exclusively in axons and neuronal processes where Abeta does most of its damage,” says Bhattacharyya, lead author of the Cell Reports paper. This role for MAMs was previously unknown, though earlier research indicated that they are increased in number and activity in the brains of people with Alzheimer’s disease.
Next, the MGH team wanted to learn what happens when MAM levels and activity were intentionally altered. They showed for the first time that preventing assembly of MAMs, either with gene therapy or a drug that blocked a key protein called the sigma-1 receptor (S1R), dramatically decreased beta secretase cleavage of palAPP in axons and lowered Abeta production. Conversely, a drug that activated S1R triggered an increase in beta secretase cleavage of palAPP and increased production of amyloid beta in axons.
“Our results suggest that the sigma-1 receptor might be a viable therapeutic target for reducing Abeta production, specifically in axons,” says Tanzi. The study also lends support for a strategy already under investigation by Tanzi and his team, which is developing an experimental treatment that inhibits the palmitoylation of APP, the process that produces palAPP. It’s also known that another class of drugs that Kovacs is studying for preventing formation of amyloid beta, called ACAT inhibitors, works directly in MAMs. In the future, these and other interventions that thwart production of this most dangerous pool of axonal amyloid beta could be used in concert with early detection (through blood or imaging tests) to stop or slow the progression of AD.
Reference: “Axonal generation of amyloid-β from palmitoylated APP in mitochondria-associated endoplasmic reticulum membranes” by Raja Bhattacharyya, Sophia E. Black, Madhura S. Lotlikar, Rebecca H. Fenn, Mehdi Jorfi, Dora M. Kovacs and Rudolph E. Tanzi, 18 May 2021, Cell Reports. DOI: 10.1016/j.celrep.2021.109134
Tanzi directs the Genetics and Aging Research Unit and co-directs the Henry and Allison McCance Center for Brain Health at MGH and is the Joseph P. and Rose F. Kennedy Professor of Neurology at Harvard Medical School (HMS). Bhattacharyya is also an instructor in Neurology at HMS.
This study was funded by grants from the National Institutes of Health and the Cure Alzheimer’s Fund.
Any one care to put that medical science speak into simple English?
Do you understand any of this?
Stay away from oranges.
Only Some, but by no means all.....................
G
Not a doctor, but it looks like they now have a good idea about how harmful, brain-damaging proteins form and this could eventually lead to effective treatments.

I think it’s about Alzheimer’s Disease.
“Any one care to put that medical science speak into simple English?”
Sure:
“...guidepost for developing new therapies...”
Translated:
We found a way to make money off of a drug which you must take to prevent the buildup of plaque, but you’re too dumb to understand that we’re taking advantage of you and withholding the information you need to prevent Alzheimer’s without our drugs.
It’s the next ‘statin’ drug, doncha know.
They discovered the mechanism by which the proteins form that cause Alzheimer’s. This should lead to therapeutics in the form of gene therapies or pills/shots that could counteract that process.
As with anything, I’m sure they’re going to test the snot out of their hypotheses, sort of like how science is supposed to work, but I don’t expect we’ll see anything for human trials for another 3-5 years.
Have not read this yet but am betting bad lipid fats from polyunsaturated vegetable oils are involved.
I am not a doctor but it sure sounds good to me.
J Biol Chem . 2005 Feb 18;280(7):5892-901. doi: 10.1074/jbc.M404751200. Epub 2004 Dec 7.
https://pubmed.ncbi.nlm.nih.gov/15590663/
Abstract
"Alzheimer's disease (AD) involves amyloid beta (Abeta) accumulation, oxidative damage, and inflammation, and risk is reduced with increased antioxidant and anti-inflammatory consumption. The phenolic yellow curry pigment curcumin has potent anti-inflammatory and antioxidant activities and can suppress oxidative damage, inflammation, cognitive deficits, and amyloid accumulation. Since the molecular structure of curcumin suggested potential Abeta binding, we investigated whether its efficacy in AD models could be explained by effects on Abeta aggregation. Under aggregating conditions in vitro, curcumin inhibited aggregation (IC(50) = 0.8 microM) as well as disaggregated fibrillar Abeta40 (IC(50) = 1 microM), indicating favorable stoichiometry for inhibition. Curcumin was a better Abeta40 aggregation inhibitor than ibuprofen and naproxen, and prevented Abeta42 oligomer formation and toxicity between 0.1 and 1.0 microM. Under EM, curcumin decreased dose dependently Abeta fibril formation beginning with 0.125 microM. The effects of curcumin did not depend on Abeta sequence but on fibril-related conformation. AD and Tg2576 mice brain sections incubated with curcumin revealed preferential labeling of amyloid plaques. In vivo studies showed that curcumin injected peripherally into aged Tg mice crossed the blood-brain barrier and bound plaques. When fed to aged Tg2576 mice with advanced amyloid accumulation, curcumin labeled plaques and reduced amyloid levels and plaque burden. Hence, curcumin directly binds small beta-amyloid species to block aggregation and fibril formation in vitro and in vivo. These data suggest that low dose curcumin effectively disaggregates Abeta as well as prevents fibril and oligomer formation, supporting the rationale for curcumin use in clinical trials preventing or treating AD." ---------------------------------------------------------------------------------------------------------------------------------
I ran across a mention turmeric/curcumin while reading "Memory Loss is not Inevitable" by Allen S Josephs, M.D. A fairly short 94 pages.
(He is a Board Certified Physican with internal medicine and neurology accreditations Previous Section Chief of nerology St Barnabas Medical Center Livinston NJ.)
India (reportedly) uses tumeric (source of curcumin) extensively in its cooking and has (reportedly) a low rate of Alzheimers.
Seems like a cheap and easy enough to incorporate in your diet pending the inevitable high cost pharmaceutical solution. Turmeric was discussed on Page 87 of the book.
I would recommend this book for anyone who has a relative who may be starting to have memory problems. (Or if you are worried at your own situation!)
And hydrogenated oils?
Dr. Tanzi has had the most significant Alz discoveries so far and if his lab says he has a breakthrough this is very good news. He is also an interesting man. This article states that Tanzi believes he knows how AB is formed in the brain. AB “may” be important as the cause of Alz formation. By knowing the AB trigger this could lead to future treatments...there is currently no successful treatment for ALZ (regardless of the recent approval by the FDA of an ALZ treatment.)Please accept that my description is written by a layman
Thanks for posting! We have a national problem with alzheimers right now!
One thing it isn't is that for anyone dealing with Alzeimer's in their home or life it doesn't make a very damn good joke.
Yup, either or both. Bad lipids.
Disclaimer: Opinions posted on Free Republic are those of the individual posters and do not necessarily represent the opinion of Free Republic or its management. All materials posted herein are protected by copyright law and the exemption for fair use of copyrighted works.