Posted on 07/02/2025 12:19:36 PM PDT by Red Badger
Abstract
Neurovascular compression (NVC) of the auditory vestibular nerve (AVN) may be one of the causes of intractable dizziness and characteristic tinnitus, which are often described as typewriter-like tinnitus. While these symptoms can be alleviated by oral administration of carbamazepine (CBZ), no standard diagnostic and surgical indications and treatment methods have been established. Microvascular decompression (MVD) is effective for these disorders. We describe two cases where MVD resulted in favorable clinical outcomes, and we also review the relevant literature. Our experience suggests that MVD may be an effective treatment option for patients who exhibit a positive response to CBZ, show clear radiological evidence of NVC, and present with both tinnitus and vertigo.
Introduction
Neurovascular compression (NVC) of the auditory vestibular nerve (AVN) is considered a possible cause of intractable dizziness and tinnitus [1,2]. The main symptoms of these disorders are severe tinnitus that can be described as “typewriter-like” and frequent vertigo [3-6]. Despite the growing recognition of this condition, standardized diagnostic criteria and treatment algorithms remain lacking. In this context, microvascular decompression (MVD) has been applied, though surgical indications are less clearly defined than for other cranial nerve compression syndromes such as trigeminal neuralgia or hemifacial spasm [4-10]. We report two cases of AVN compression with favorable outcomes following MVD. Both cases met the criteria involving a specific clinical triad: responsiveness to carbamazepine (CBZ), radiological evidence of vascular compression in the internal acoustic canal (IAC), and the presence of both vertigo and characteristic tinnitus. We also engage in a review of the relevant literature and discuss surgical strategies. These cases provide further insights into the diagnostic and therapeutic approach to this uncommon but disabling condition.
Case Presentation
Case 1
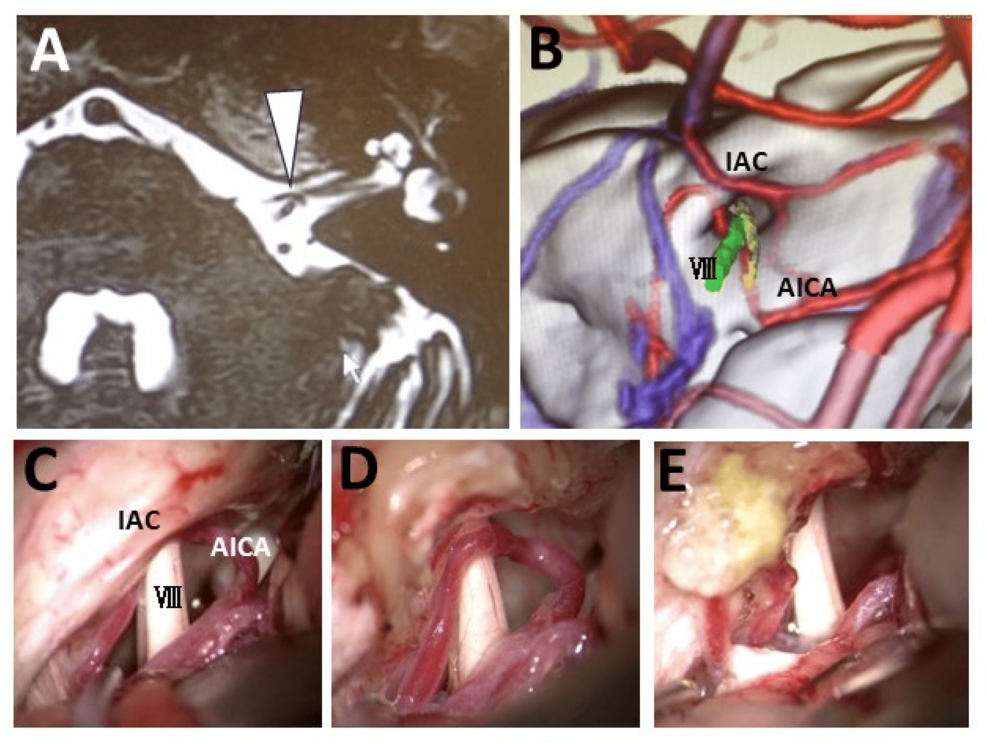
The patient was a 58-year-old male who had suffered from progressive vertigo accompanied by left pulsatile tinnitus lasting approximately 10-30 seconds for the past six years. An MRI performed at a local internal medicine clinic had detected no abnormalities. He had been diagnosed with neuromodulated syncope and was treated conservatively. However, his symptoms had worsened, and hence, he had been referred to our department with suspicion of NVC of the AVN. The auditory brainstem response (ABR) was within the normal range. The caloric test showed decreased left-sided response. Constructive interference in steady state (CISS) MRI and 3D CT angiography-venography revealed a vascular loop of the anterior inferior cerebellar artery (AICA) extending into the internal auditory meatus (IAM) and compressing the vestibular portion of the eighth cranial nerve (Figures 1A, 1B). The symptoms improved with oral administration of CBZ. However, the symptoms did not completely disappear despite increasing the medication to the maximum dosage. Therefore, MVD of the eighth cranial nerve was performed. The intraoperative findings corresponded precisely with the preoperative imaging (Figures 1C, 1D), further validating the surgical plan, and transposition of the AICA was performed (Figure 1E). Intraoperative ABR monitoring showed no abnormalities. The postoperative course was uneventful, and the symptoms completely disappeared. No recurrence has been observed in the subsequent three years.
Preoperative-imaging-and-intraoperative-field-images-of-Case-1
Figure 1: Preoperative imaging and intraoperative field images of Case 1
A: Preoperative head CISS MRI showing the left elongated AICA forming a loop within the IAC and compressing the vestibular nerve (VIII) at the internal acoustic meatus (white arrowhead). B: Fusion image of 3D CT angiography and head MRI showing the AICA compressing the vestibular nerve. C–E: Intraoperative findings confirming cranial nerve compression by the AICA after opening the internal acoustic meatus (C and D), and hence transposition of the AICA was performed (E)
AICA: anterior inferior cerebellar artery; CISS: constructive interference in steady state; CT: computed tomography; IAC: internal acoustic canal; MRI: magnetic resonance imaging
Case 2
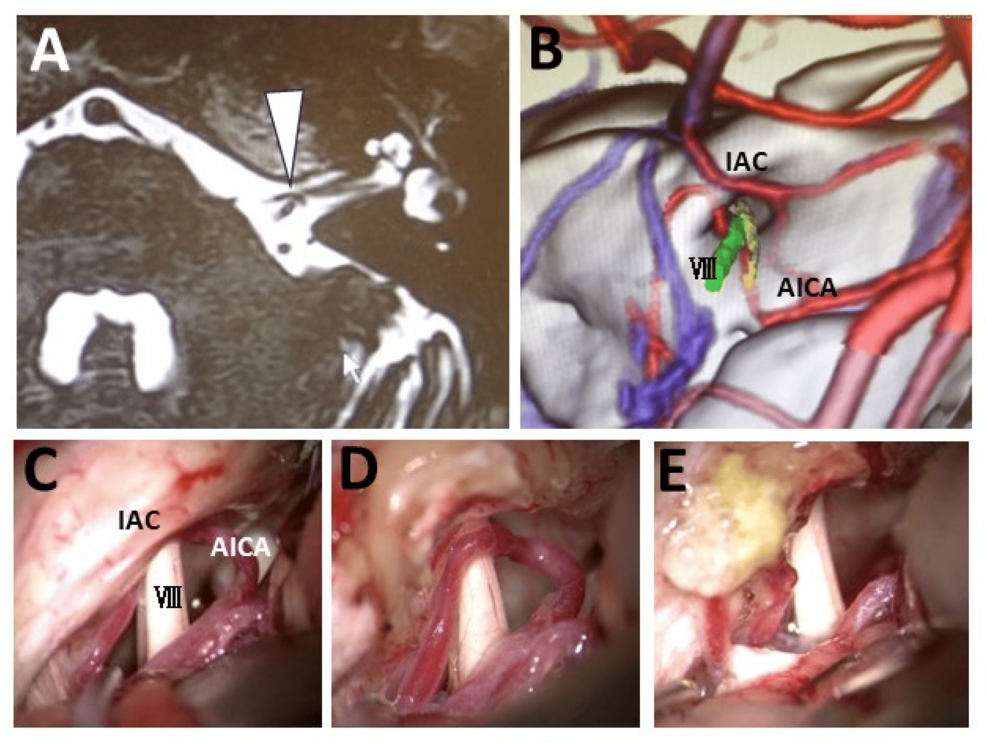
The patient was a 46-year-old male who had suffered from progressive left pulsatile tinnitus for the past eight years. Severe vertigo had started to synchronize with the tinnitus for four years. As his symptoms had worsened, he had suffered refractory tinnitus accompanied by severe vertigo dozens of times per day. He had been referred to our department with suspicion of NVC of the AVN. CISS MRI and 3D CT angiography-venography showed compression of the left eighth cranial nerve by the AICA in the IAM (Figures 2A, 2B). The symptoms improved with oral administration of CBZ. However, continued oral medication with CBZ became difficult due to the strong side effects such as nausea and vomiting. Therefore, MVD of the eighth cranial nerve was performed. Intraoperative findings confirmed AICA compression of the eighth nerve after opening the IAM, and hence, transposition of the AICA was performed (Figures 2C, 2D). The strong correlation between imaging and operative findings reinforced the value of high-resolution preoperative imaging in surgical planning. Intraoperative ABR monitoring showed no abnormalities. The postoperative course was uneventful, and the symptoms completely disappeared.
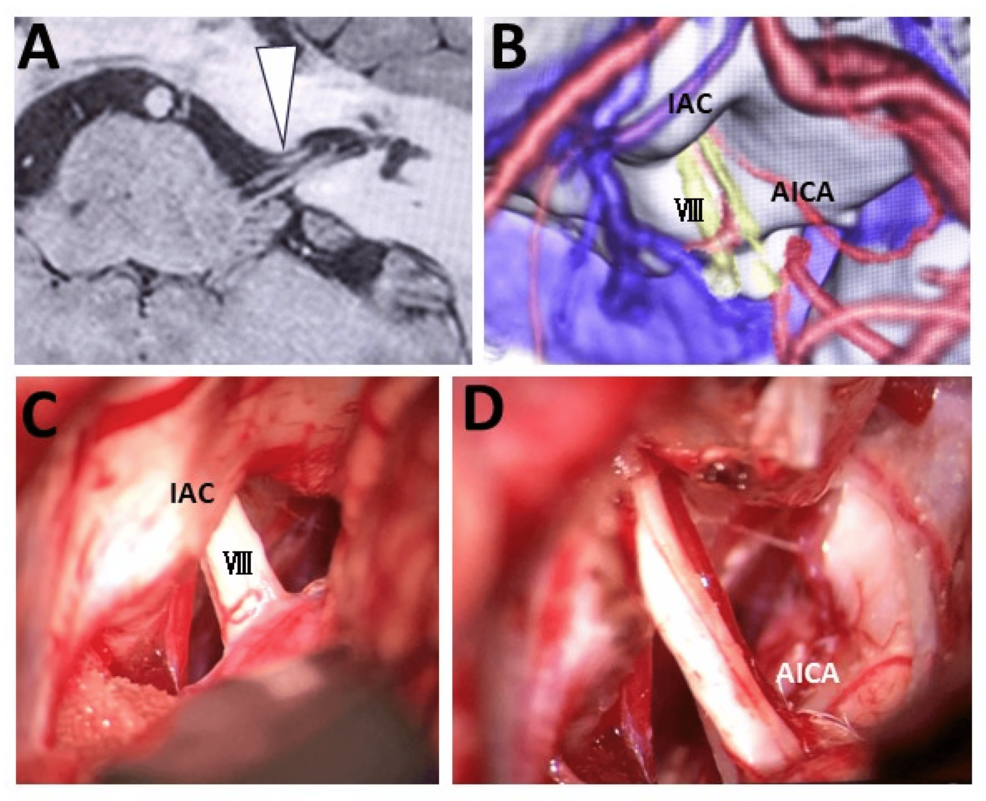
Preoperative-imaging-and-intraoperative-field-images-of-Case-2
Figure 2: Preoperative imaging and intraoperative field images of Case 2
A: Preoperative head CISS MRI showing the left elongated AICA forming a loop within the IAC and compressing the vestibular nerve (VIII) at the internal acoustic meatus (white arrowhead). B: Fusion image with 3D CT angiography-venography showing the direction of compression by the offending artery and relationships between the anatomical components. C, D: Intraoperative findings confirming cranial nerve compression by the AICA after opening the internal acoustic meatus; hence, transposition of the AICA was performed
AICA: anterior inferior cerebellar artery; CISS: constructive interference in steady state; CT: computed tomography; IAC: internal acoustic canal; MRI: magnetic resonance imaging
Discussion
Pathophysiology of symptoms caused by NVC
Cerebral vessels may elongate due to aging or atherosclerosis, or become narrower compared to normal; however, as the volume of the posterior fossa remains unchanged, the vessels gradually curve and meander [11,12]. The neuroprotective effect of the nerve sheath is physically vulnerable at the transposition point between the central myelin and peripheral myelin at the brainstem. Therefore, symptoms may occur if a vessel contacts and compresses the myelin sheath transition point [1]. The location of the vulnerable myelin sheath zone varies, the closest to the root exit zone for the glossopharyngeal and vagus nerves at about 2 mm from the brainstem, for the facial nerve at 3 mm, for the trigeminal nerve at 4 mm, and the AVN has a very wide range of 10 mm [1]. Therefore, NVC may affect even the distal side of the AVN. Neuroimaging findings have also suggested that NVC near the IAC will likely induce symptoms [13]. The offending vessels, which curve and meander, initially contact the cranial nerves, but symptoms will presumably develop as the cranial nerves are gradually compressed and displaced, causing nerve damage at the physically vulnerable myelin transition area. In particular, as the offending vessels elongate into the narrow space at the IAC, the compression pressure on the AVN will become greater.
Effectiveness of MVD
The effectiveness rate of MVD for NVC is 83% for trigeminal neuralgia, 91% for hemifacial spasm, and 92% for glossopharyngeal neuralgia [7,8]. On the other hand, the effectiveness rate is lower compared with trigeminal neuralgia and hemifacial spasm: improvement in symptoms of tinnitus was 28%, that in vertigo was 32%, and that in tinnitus and vertigo was 62% [4,5]. The lower effectiveness rate of MVD for AVN reflects the uncertainty of the surgical indication, including MVD's ineffectiveness in cases such as those refractory to CBZ oral administration and/or those with no offending artery on the neuroimaging findings. This ineffectiveness might be affected by long disease duration. Even if MVD is performed more than four years after the onset of symptoms, irreversible neurological damage may have occurred [14]. Therefore, MVD should be performed within the appropriate period, as delays might cause the surgical effect to be weakened due to irreversible damage caused by NVC. Careful patient selection plays an important role in optimizing surgical outcomes. Based on our case reports and a review of the literature, patients who present with both vertigo and characteristic "typewriter-like" tinnitus demonstrate partial improvement with CBZ, and show radiological evidence of neurovascular compression within the IAC, could potentially benefit from MVD.
Surgical strategy and intraoperative monitoring
The compression site by the offending vessels is often located at the peripheral site of the cranial nerve, often within the IAM; hence, opening of the IAC will be necessary to confirm the compression site in the IAM. Both our patients required opening of the IAM to confirm the compression site. Removal of the posterior wall of the IAM by bone drilling requires care to avoid involving the surrounding cranial nerves and cerebral vessels passing through the region. If mastoid air cells have developed up to the posterior wall of the IAM, postoperative cerebrospinal fluid leakage is a risk due to the opening of the mastoid air cells by bone drilling; hence, adequate coating with bone wax and/or fascia is necessary. The AICA will often be the responsible blood vessel. Transposition of the offending AICA requires care that blood flow in its branch, the subarcuate artery, which runs into the IAM, is not obstructed. Full use of the birdlime technique, “a sutureless method that employs a fibrin glue-soaked TachoSil® sheet to secure the transposed vessel in place without damaging surrounding structures,” is necessary to perform such a reliable vascular transposition [15-17].
Complications of MVD for vestibular auditory nerves include hearing dysfunction and brainstem infarction caused by perforator damage. Hearing dysfunction can be caused by tension on the auditory nerve due to brain traction and impaired blood flow in the subarcuate artery during transposition, which can be prevented by continuous intraoperative monitoring of the ABR. We usually perform indocyanine green video-angiography to prevent brainstem infarction caused by perforator damage. However, the perforators behind the surgical field cannot be confirmed. Therefore, motor evoked potential and sensory evoked potential can be useful to confirm the obstruction of these perforators. Intraoperative neurological monitoring is essential for safely completing MVD under these conditions.
Conclusions
Although no standard surgical treatment has been established for AVN compression, our cases suggest that MVD can be effective in selected patients. Favorable outcomes may be achieved when specific criteria are met, namely, symptom relief with CBZ, radiological evidence of NVC within the IAC, and the presence of both vertigo and characteristic tinnitus. Safe and reliable surgical outcomes depend on appropriate patient selection and meticulous techniques, including decompression within the IAC and intraoperative monitoring. Further case accumulation is necessary to refine indications and improve long-term results.
References
Guclu B, Sindou M, Meyronet D, Streichenberger N, Simon E, Mertens P: Cranial nerve vascular compression syndromes of the trigeminal, facial and vago-glossopharyngeal nerves: comparative anatomical study of the central myelin portion and transitional zone; correlations with incidences of corresponding hyperactive dysfunctional syndromes. Acta Neurochir (Wien). 2011, 153:2365-75. 10.1007/s00701-011-1168-1
Bergsneider M, Becker DP: Vascular compression syndrome of the vestibular nerve: a critical analysis. Otolaryngol Head Neck Surg. 1995, 112:118-24. 10.1016/S0194-59989570310-1
Mathiesen T, Brantberg K: Microvascular decompression for typewriter tinnitus-case report. Acta Neurochir (Wien). 2015, 157:333-6. 10.1007/s00701-014-2324-1
van den Berge MJ, van Dijk JM, Posthumus IA, Smidt N, van Dijk P, Free RH: Microvascular decompression of the cochleovestibular nerve for treatment of tinnitus and vertigo: a systematic review and meta-analysis of individual patient data. J Neurosurg. 2017, 127:588-601. 10.3171/2016.8.JNS16992
Jannetta PJ, Møller MB, Møller AR, Sekhar LN: Neurosurgical treatment of vertigo by microvascular decompression of the eighth cranial nerve. Clin Neurosurg. 1986, 33:645-65.
Møller MB, Møller AR, Jannetta PJ, Jho HD, Sekhar LN: Microvascular decompression of the eighth nerve in patients with disabling positional vertigo: selection criteria and operative results in 207 patients. Acta Neurochir (Wien). 1993, 125:75-82. 10.1007/BF01401831
Zakrzewska JM, Linskey ME: Trigeminal neuralgia. BMJ. 2014, 348:g474. 10.1136/bmj.g474
Miller LE, Miller VM: Safety and effectiveness of microvascular decompression for treatment of hemifacial spasm: a systematic review. Br J Neurosurg. 2012, 26:438-44. 10.3109/02688697.2011.641613
Yap L, Pothula VB, Lesser T: Microvascular decompression of cochleovestibular nerve. Eur Arch Otorhinolaryngol. 2008, 265:861-9. 10.1007/s00405-008-0647-3
Zhang L, Yu Y, Yuan Y, Xu J, Xu X, Zhang J: Microvascular decompression of cochleovestibular nerve in patients with tinnitus and vertigo. Neurol India. 2012, 60:495-7. 10.4103/0028-3886.103194
Park SH, Hwang SK, Lee SH, Park J, Hwang JH, Hamm IS: Nerve atrophy and a small cerebellopontine angle cistern in patients with trigeminal neuralgia. J Neurosurg. 2009, 110:633-7. 10.3171/2008.8.JNS08522
Rasche D, Kress B, Stippich C, Nennig E, Sartor K, Tronnier VM: Volumetric measurement of the pontomesencephalic cistern in patients with trigeminal neuralgia and healthy controls. Neurosurgery. 2006, 59:614-20. 10.1227/01.NEU.0000228924.20750.D4
Haller S, Etienne L, Kövari E, Varoquaux AD, Urbach H, Becker M: Imaging of neurovascular compression syndromes: trigeminal neuralgia, hemifacial spasm, vestibular paroxysmia, and glossopharyngeal neuralgia. AJNR Am J Neuroradiol. 2016, 37:1384-92. 10.3174/ajnr.A4683
De Ridder D, Vanneste S, Adriaenssens I, et al.: Microvascular decompression for tinnitus: significant improvement for tinnitus intensity without improvement for distress. A 4-year limit. Neurosurgery. 2010, 66:656-60. 10.1227/01.NEU.0000366110.87836.53
Otani N, Toyooka T, Fujii K, et al.: "Birdlime" technique using TachoSil tissue sealing sheet soaked with fibrin glue for sutureless vessel transposition in microvascular decompression: operative technique and nuances. J Neurosurg. 2018, 128:1522-9. 10.3171/2017.1.JNS161243
Otani N, Toyooka T, Takeuchi S, Tomiyama A, Wada K, Mori K: Novel technical variations and increased adhesive strength in the "birdlime" transposition technique for microvascular decompression. World Neurosurg. 2018, 116:e460-8. 10.1016/j.wneu.2018.05.006
Mori K, Otani N, Toyooka T, Morita S, Numazawa S, Wada K, Watanabe S: Validation of efficacy and safety of TachoSil® tissue sealant for vessel transposition in microvascular decompression. Oper Neurosurg (Hagerstown). 2023, 25:417-25. 10.1227/ons.0000000000000844
CAN YOU HEAR ME NOW?????...............
PING!.....................
Prog Rock album from 1975.
Dude, I have the eight track.
By Alice Cooper...............
Anyone who has tinnitus needs to check their panoramic XRAY to see if they have Eagle Syndrome. The spikes in your head/neck can create problems.
Don’t count on anyone, including dentists, to diagnose this for you. Look for yourself.
I have had a 3d CISS MRI. It came back not showing a problem with nerves. However, I can change my tinnitus when it ratchets up by moving my head - especially when laying down.
Pulsatile tinnitus is very much unlike other forms of tinnitus in that you are actually hearing real internal sounds, such as your blood flow.
Not sure why the study doesn't clarify that.
Anyone have these symptoms should have a MRI asap as it could be an Acoustic Neuroma as I had the same symptoms. I have had two tumors as in spite of the claim more and more people are getting them...Also had horrible nose bleeds, never ending headaches, loss of hearing, Vertigo and Tinnitus to name a few. Mine was a fast growers and nearly killed me, I had Vertigo so bad I could not walk a straight line and Tinnitus was so loud in my head I had to sleep with a radio blaring at full volume in order to sleep. I had the first one cut out involving a 16 hr surgery and 2nd had 8 radiation treatments. Luckily I had the Doctors cut my vestibulocochlear nerve as I had researched it as any disturbance to the hearing nerves could result in life long Tinnitus so better to be deaf than that so afterwards I got a implant minus the Tinnitus.
BKMK
Cool. Now do it without surgery.
Bookmark
Bookmark
BKMK
I have tinnitus, not nearly as bad a you, but I have also had three episodes of vertigo in the last three years. Bad enough that I couldn’t walk a straight line or almost fall over. Luckily I didn’t and they only lasted a few days. I did tell my doctor who ordered an MRI. Nothing was found. It’s gonna happen again, just a matter of when. It doesn’t just happen-I wake up with it.
Disclaimer: Opinions posted on Free Republic are those of the individual posters and do not necessarily represent the opinion of Free Republic or its management. All materials posted herein are protected by copyright law and the exemption for fair use of copyrighted works.