Located in the back of our abdomen, the pancreas is a long flattened organ and gland that is part of both our digestive and endocrine systems. The two main functions pancreas has are producing enzymes to help with digestion and sending the hormone insulin (among others) to control the blood glucose level in the body.
Pancreatic cancer is a disease in which malignant cells form in the tissues of the pancreas. It is the most lethal of cancers, with a current overall five-year survival rate of approximately 7 percent. At the moment, it is the fourth most common cause of cancer deaths in the United States. And according to board-certified oncologist Dr. Brian Geister, Pancreatic cancer will become the leading cause of cancer deaths in America by 2030.
According to estimates of the American Cancer Society, in 2022, around 62,210 people will be diagnosed with pancreatic cancer, and approximately 49,830 people will die from it.
Why Is Pancreatic Cancer So Deadly?
According to Rachna T Shroff, MD, MS, an associate professor of medicine and chief of GI medical oncology at the University of Arizona Cancer Center, pancreatic cancer is considered a deadly disease for several reasons. First, since it doesn’t produce a lot of specific symptoms, it is seldom detected in early stages when it is the most curable. Its symptoms only surface after it has spread to other organs. Therefore, around 80 percent of patients present with advanced stages. She further explained that “advanced” means that the cancer is locally advanced and cannot be removed surgically, or it has metastasized to other organs. The disease’s tendency to metastasize to other parts of the body is the second reason why it is so lethal.
Major Causes of Pancreatic Cancer
Pancreatic cancer is caused by DNA mutations which take place due to genetic predispositions, lifestyle factors such as alcohol consumption and smoking, or can occur by coincidence.
Inherited mutations: Such individuals inherit a mutant gene copy from one of their parents. With a genetic predisposition, their risk of developing pancreatic cancer is higher than that of people without the mutant gene. However, not every one of them will get cancer. As they age, the good gene copy of a cell in the pancreas may become damaged, and thus they end up with two damaged genes. And as a result, that cell will grow abnormally and possibly form pancreatic cancer.
Lifestyle factors: Smoking and alcohol consumption can cause pancreatic cancer. People who smoke are two to three times more likely to develop this disease than those who don’t. Also, chronic and heavy alcohol consumption can lead to repeated inflammation of the pancreas, which in turn can result in pancreatic cancer.
Chance occurrence: When a cell in our body divides, it copies all of its DNA for the new cell. Our body is constantly copying DNA and making new cells. However, mistakes do happen in copying DNA. And if one of these mistakes damages a key cancer-associated gene in a pancreatic cell, then a cancer may form as a result.
Many pancreatic cancer cases are by chance, although many genes play a role in its development. The major driver genes of pancreatic cancer include KRAS, P53, P16, and SMAD4.
Early Signs and Symptoms of Pancreatic Cancer
One of the largest challenges the medical community faces is the detection of pancreatic cancer in its early stages. There are no telltale signs for pancreatic cancer, and its symptoms are non-specific and similar to those of other diseases.
Common symptoms of pancreatic cancer may include:
- Painless jaundice: Yellowing of the skin and the whites of the eyes can occur when the tumor in the head of the pancreas blocks the bile duct
- Abdominal pain that extends to the back
- Loss of appetite
- Weight loss for unknown reasons
- Pale and greasy stools
- Dark-colored urine
- Itchy skin
- New diagnosis of diabetes or existing diabetes that’s becoming more difficult to control
- Venous thrombosis
- Fatigue
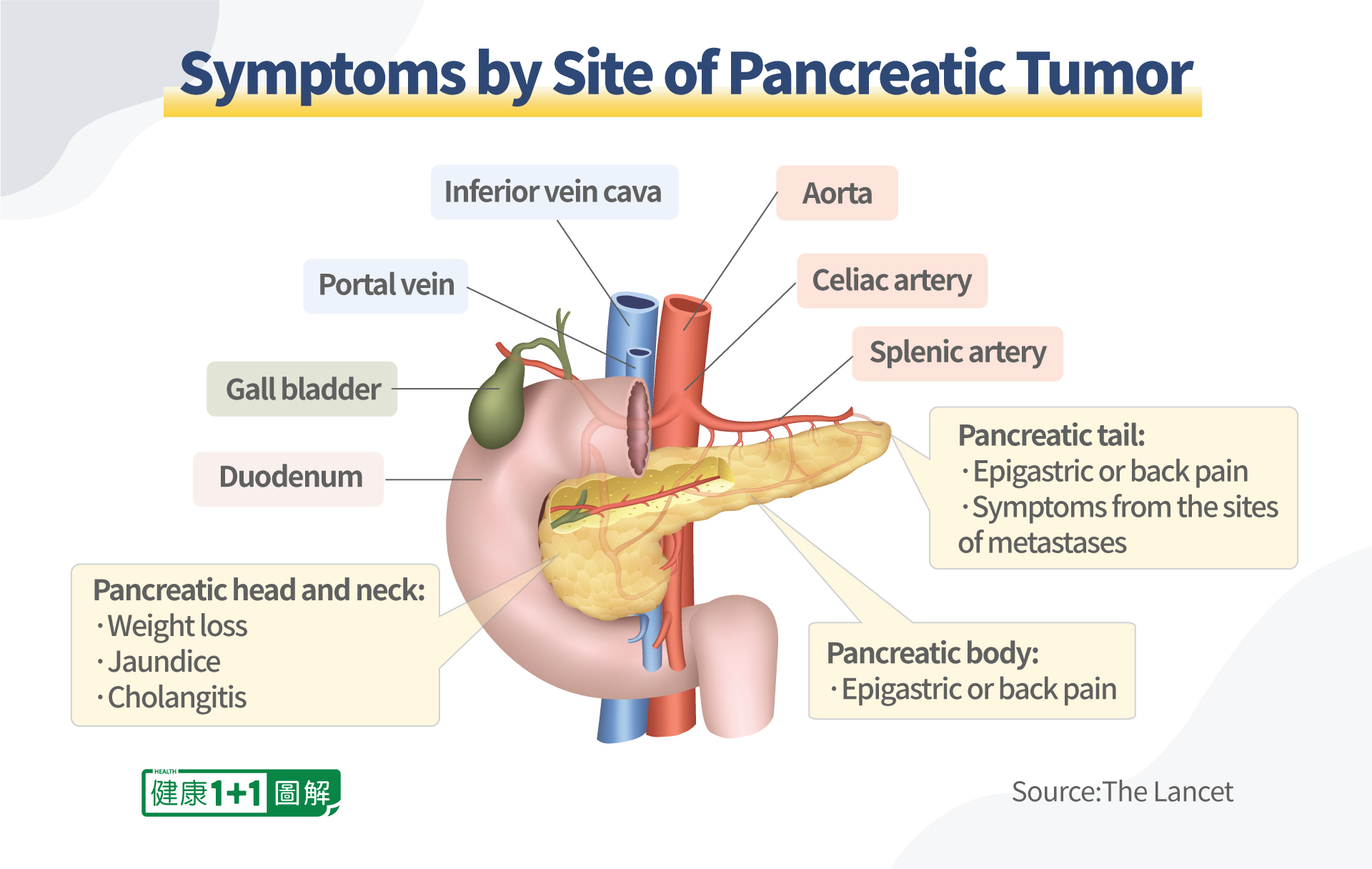
According to Dr. Shroff, symptoms of pancreatic cancer depend on the primary tumor’s location in the pancreas. For instance, if the tumor is located in the head or neck of the pancreas, the patient may experience weight loss, jaundice, or cholangitis. Since the common bile duct that drains the entire biliary tree runs through the head of the pancreas, in patients who have pancreatic head tumors, one of the first things that happens is obstruction or blockage of that common bile duct. This is why pancreatic head tumors are more prone to presenting with jaundice.
If the tumor is in the pancreatic body, the patient may have epigastric or back pain. The pain issues are really related to anatomy of the region as there is a whole rich nerve supply running up and down the blood vessels that run through the abdomen, including the celiac plexus. Therefore, the tumor’s location determines which nerves are triggered, and it also often determines where the pain is. In addition to back pain from tumors located in the tail of the pancreas, the patient may have the symptoms from other parts of the body to which the pancreatic cancer has metastasized.
As we can see, symptoms such as weight loss, abdominal pain, itchy skin, and fatigue can be caused by many other diseases. So, often before someone finally thinks of doing a CT scan or having other tests for pancreatic cancer, it’s already too late.
Risk Factors of Pancreatic Cancer
Unfortunately, most pancreatic cancer cannot be prevented and the average lifetime risk of pancreatic cancer is about 1 in 64. However, we can try to avoid many of the controllable risk factors that increase our chances of developing pancreatic cancer.
Controllable risk factors include:
- Smoking: Around 25 percent of pancreatic cancer cases are believed to have been caused by cigarette smoking. Cigar smoking and even the use of smokeless tobacco products can also increase risk.
- Obesity: People who are obese have a 20 percent greater risk of developing pancreatic cancer than people with normal weight. And the risk is also greater for people of normal weight but with extra weight at their waistline.
- Alcohol consumption: Heavy alcohol consumption can lead to chronic pancreatitis, which can be a precursor of pancreatic cancer.
- Diet: Some foods contain vitamins, minerals, and other nutrients which can lower pancreatic cancer risk.
- Chemicals: Exposure to chemicals such as pesticides and petrochemicals may increase risk for pancreatic cancer.
Uncontrollable risk factors include:
- Age: The older one gets, the higher the risk of pancreatic cancer. Ninety percent of patients are older than 55, and 70 percent are older than 65.
- Gender: More men develop pancreatic cancer than women.
- Ethnicity: Black people are more likely to develop pancreatic cancer than Caucasian, Hispanic, or Asian people.
- Family history: People with inherited genetic mutations are at increased risk for pancreatic cancer. Specifically, an individual may be at an increased risk if two or more of his first-degree relatives or at least three members of his family have been diagnosed with pancreatic cancer.
Pancreatic Cancer in Relation to Other Diseases
Many studies have indicated that people with diabetes, especially long-term, are at an increased risk of developing pancreatic cancer. Other clinical trials have found that people with new-onset diabetes, specifically those who suddenly develop diabetes later in adulthood, are most likely to have pancreatic cancer. However, diabetes is still much more common than pancreatic cancer and not all people with diabetes will develop pancreatic cancer.
Also, some genetic syndromes can cause pancreatic cancer, such as the hereditary breast and ovarian cancer syndrome. This syndrome is caused by BRCA mutations.
There is a proven relationship between BRCA mutations and pancreatic cancer. A BRCA mutation approximately doubles the lifetime risk of developing pancreatic cancer. Nevertheless, breast cancer is also much more common than pancreatic cancer.
According to one study, people with a previous hepatitis B infection have an increased risk of developing pancreatic cancer.
Current Treatments for Pancreatic Cancer
Currently, treatments for pancreatic cancer can be any combination of the five types of standard treatment, including surgery, chemotherapy, and radiation procedures.
- Surgery: used to remove the pancreatic tumor.
- Radiation therapy: uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
- Chemotherapy: uses drugs to stop the growth of cancer cells, and it is one of the most commonly used treatment method for pancreatic cancer.
- Chemoradiation therapy: a combination of chemotherapy and radiation therapy
- Targeted therapy: uses drugs or other substances to identify and attack specific cancer cells, while trying to minimize harm to normal cells.
However, pancreatic cancer is significantly more resistant to chemotherapy in comparison to other cancers. Therefore, patients with pancreatic cancer are presented with fewer options than patients with other kinds of cancers.
According to Dr. Shroff, the mainstay of treatment for advanced pancreatic cancer remains chemotherapy, such as FOLFIRINOX, a chemotherapy regimen using four medications, including folinic acid, fluorouracil, irinotecan, and oxaliplatin. Another common chemotherapy regimen uses the drugs gemcitabine plus nab-paclitaxel which have been shown in some studies to increase pancreatic cancer survival rate.
Dr. Shroff said that there are subsets of patients that have other options. For instance, for patients who have pancreatic cancer associated with a BRCA mutation. If after being initially treated with certain types of chemotherapies that involve oxaliplatin or cisplatin, and if they are responsive to those treatments, may be eligible for a targeted therapy using a PARP inhibitor. PARP inhibitors are a group of pharmacological inhibitors of the enzyme poly ADP ribose polymerase, and they’re FDA-approved for treating a lot of BRCA mutated cancers, including pancreatic cancer as an oral maintenance therapy for patients after the initial chemotherapy.
There is also a small percentage of patients that can be identified through comprehensive genomic profiling or biomarker testing, as having microsatellite instability-high cancer. These patients might be eligible for immunotherapy.
According to the Cancer Research Institute, the only treatment that can potentially cure patients with pancreatic cancer is the complete surgical removal of the pancreas. However, less than 20 percent of these patients are eligible for this operation and many will relapse after the surgery as the cancer cells have already metastasized before the operation. Furthermore, although living without a pancreas is possible, these patients will become diabetic and need to take insulin and enzyme pills regularly to help maintain a normal blood sugar level and the ability to digest food for the rest of their lives.
Emerging Immunotherapy to Treat Pancreatic Cancer
Besides the aforementioned traditional treatment methods, immunotherapy is showing promise as a less toxic pancreatic cancer treatment. Our immune system protects our body against foreign invaders, including bacteria, toxins, and viruses. However, cancer cells can play a trick on our immune system by developing genetic changes that prevent the immune cells from recognizing them as a threat. The cancer cells can then metastasize to other parts of the body while evading the immune system.
Immunotherapy uses drugs to boost our immune system to help it seek out and kill the cancer cells. Unfortunately, according to Dr. Shroff, immunotherapy currently plays a role only for a small subset of patients, approximately 3 percent of all pancreatic cancer cases, who are MSI high (aka. tumor mutation burden high).
However, many in the medical community believe that the future for treating pancreatic cancer is immunotherapy. For instance, the Johns Hopkins Hospital is testing recently developed immunotherapies in clinical trials.
There are also clinical studies that combine a PARP inhibitor with a checkpoint blockade agent. Since PARP enzymes help repair damaged cells, the PARP inhibitor instead blocks the enzymes and makes it harder for cancer cells to repair themselves.
In early 2022, a national, randomized clinical trial conducted by Perelman School of Medicine at the University of Pennsylvania and sponsored by the Parker Institute for Cancer Immunotherapy showed that a combination of chemotherapy with immunotherapy can unleash the anticancer capacity of the immune system against pancreatic cancer. The trial results were subsequently published in Nature Medicine.
The small-scale trial had 34 participants who were patients with advanced pancreatic cancer. They were randomized to receive the immunotherapy nivolumab with two chemotherapy drugs, nab-paclitaxel and gemcitabine. Their one-year survival rate improved from the average of 35 percent with chemotherapy alone to be 57.7 percent, which is significantly greater.
An initial small clinical trial conducted by the team of Dr. Robert Vonderheide, director of the Abramson Cancer Center at the University of Pennsylvania, in 2021 suggested that chemotherapy can substantially disrupt pancreatic tumors’ resistance to immunotherapy, thus making the treatment combination more effective. Dr. Vonderheide’s team are now planning to test this approach on a larger scale.
According to Dr. Shroff, there is much ongoing research trying to figure out how to make a cold tumor, one which is not normally sensitive to immunotherapy, more immune responsive. Some data suggest that certain immunotherapy combinations can make the immune microenvironment a little bit more responsive to the traditional immune therapies, like the checkpoint inhibitors. All of this is in clinical trial format right now. And also, there are the CAR T cellular therapies (CT), which require a very clear target. Although there is not an obvious target that is present in most patients with pancreatic cancer, the medical community is getting better at identifying some of those potential targets and developing cellular therapies around them as well.
Is It Possible to Survive Pancreatic Cancer in the Long Term?
Despite the dismal survival rate for pancreatic cancer, there are long-term survivors, and it is even possible to make a full recovery.
Dr. Shroff finds it incredibly rewarding to be able to see her long-term survivor patients live the best life and meet milestones. Some of her patients underwent surgical resection and curative resection several years, even ten years ago.
For instance, a young father of two was diagnosed with pancreatic cancer around seven years ago, and he underwent surgery and chemotherapy, and has been able to watch his children grow up. Another patient, who has been on chemotherapy and nab-paclitaxel for almost four years, is still traveling and hiking regularly in the mountains with his wife and spending time with his kids. And in 2011, he celebrated his daughter’s wedding. For Dr. Shroff, the purpose of cancer treatment is not only prolonging a patient’s life, but giving him or her the best quality of life.
In Dr. Shroff’s opinion, cancer has a tendency to be a “wake-up call” for some patients. As a result, they do all the things in their control to fight the disease and feel better, such as modifying their diet. Some of them create a bucket list to do the things that they really want to do, see the people they want to see, and visit the places they want to visit. A lot of her patients have reprioritized and restructured their life to ensure that they are living every day to its fullest and enjoying and appreciating every moment they have. And this is also a reminder for her, to never take anything for granted.
Ways to Reduce Pancreatic Cancer Risk
Unfortunately, most pancreatic cancer cases cannot be prevented. However, we can reduce our risk of developing this disease by avoiding the aforementioned risk factors.
According to Dr. Shroff, the things in our control are all lifestyle-related. For instance, in order to reduce the risk, people should quit smoking, maintain a healthy weight, keep a well-balanced diet rich in fruits, vegetables, and lean meats to avoid diabetes and limit their alcohol intake.
Also, since about 3 percent to 5 percent of pancreas cancers are caused by inherited or germline mutations, if someone has a family history of cancer, it’s really important for him or her to undergo genetic testing and cancer screening.
There has been a lot of effort focused on early diagnosis and or screening modalities for pancreatic cancer. Currently, there are no simple tests for pancreatic cancer. Nevertheless, there is active research at Johns Hopkins aimed at developing a test for pancreatic cancer in the blood, urine, and stool.
According to Dr. Shroff, the studies to date that have looked at screening either with radiographic approaches or endoscopic approaches have not demonstrated a dramatic survival benefit, except in potentially high risk patients that have germline or inherited mutations. However, there are a lot of exciting technologies in the liquid biopsy space. Liquid biopsy is a test performed to detect cancer by collecting and analyzing biomarkers from cancer cells in the peripheral blood. So early detection through identifying circulating tumor DNA or cell-free DNA is all accessible via simple blood draws.
Similar to other cancers, early detection of pancreatic cancer can lead to the best long-term outcomes. When detecting pancreatic cancer, the following tests and procedures may be used:
- Physical exam and health history examination
- CT scan (CAT scan): Also called computed axial tomography, this procedure makes a series of detailed pictures of the pancreas.
- MRI (magnetic resonance imaging): This procedure also makes a series of detailed pictures of the pancreas by using a magnet and radio waves.
- Blood chemistry studies: A blood sample is checked to measure the amounts of certain substances, and an unusual amount of a particular substance can be a sign of disease.
- Tumor marker test: Similar to blood chemistry studies, this procedure examines a sample of blood, urine, or tissue to measure the amounts of certain substances, which are called tumor markers.
- PET scan (positron emission tomography scan): This procedure is used to find malignant tumor cells in the pancreas.
- Ultrasound: This is using sound waves to examine structures in the body.
- Endoscopic ultrasound (EUS): An endoscope can be inserted into the body to bounce high-energy sound waves off the pancreas to make echoes, which will form a picture of pancreatic tissues.
- Laparoscopy: This is a surgical procedure to check for signs of disease in the pancreas, by making small cuts on the abdominal wall and inserting a laparoscope through the cuts to visualize the pancreas and take detailed pictures.
- Biopsy: The checking of removed cells or tissues under a microscope for signs of pancreatic cancer.
As pancreatic cancer can interfere with the production of pancreatic enzymes and hormones, a patient’s food digestion and overall quality of life will be negatively affected. However, certain foods and dietary habits can help patients fight against pancreatic cancer:
- Consuming six to eight small and well-balanced meals at regular intervals can improve the patient’s energy level.
- Staying hydrated throughout the day: It is recommended to drink eight 8-ounce glasses of water per day.
- Avoiding sugars, carbohydrates, and fats in meals to help keep a stable blood sugar level and reduce the pancreas’s burden.
- Having high-protein foods in every meal: High protein foods include lean meats (poultry and fish), tofu, beans, eggs, and nut butters.
- Eating foods that are easy to digest
- Consuming at least five servings of fruits and vegetables per day, as they are high in antioxidants, which can help fight pancreatic cancer.