Posted on 02/01/2022 5:35:25 AM PST by Red Badger
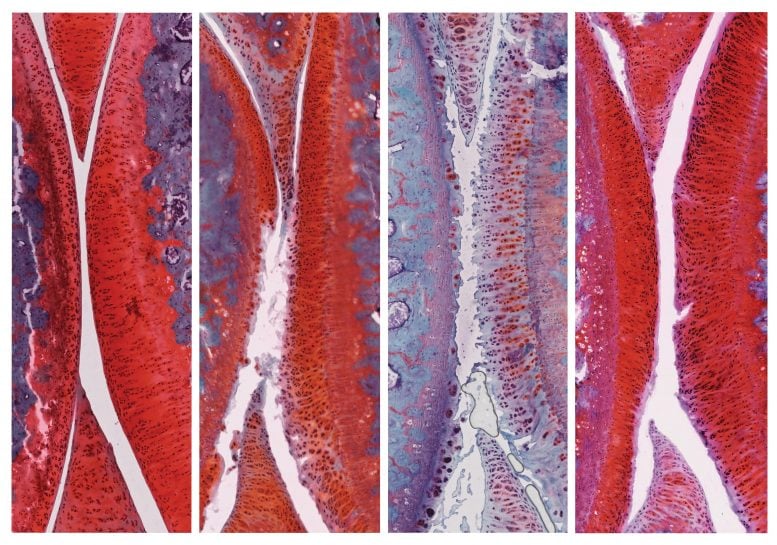
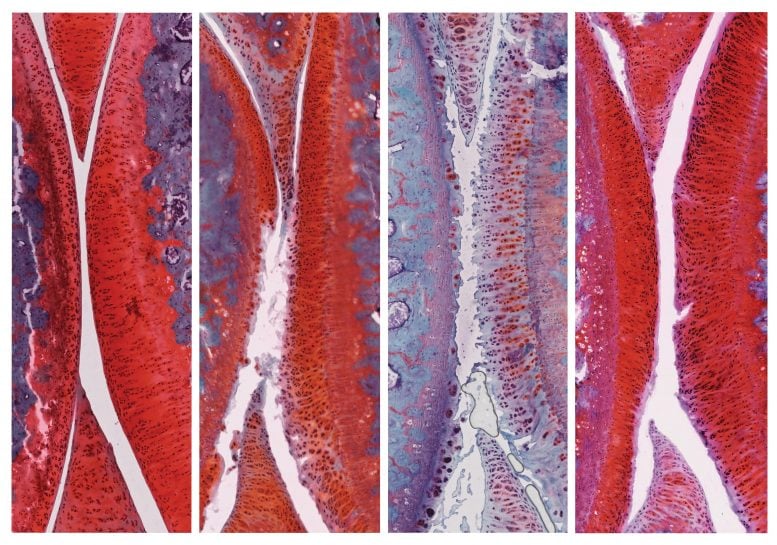
The left image shows a knee joint in a healthy rat. (White indicates cartilage.) The second image from the left shows a joint with grade 2 untreated osteoarthritis. The third image shows a joint with osteoarthritis that has worsened from grade 2 to grade 4 after six weeks of placebo therapy. The right image shows a joint with osteoarthritis that improved from grade 2 to grade 1 (mild) after six weeks of combination therapy with alphaKlotho and sTGFbR2. Credit: Salk Institute
*****************************************************************
A combination of two previously studied osteoarthritis drugs works better than either drug alone.
People with osteoarthritis, or “wear and tear” arthritis, have limited treatment options: pain relievers or joint replacement surgery. Now, Salk researchers have discovered that a powerful combination of two experimental drugs reverses the cellular and molecular signs of osteoarthritis in rats as well as in isolated human cartilage cells. Their results were published in the journal Protein & Cell on January 16, 2020.
“What’s really exciting is that this is potentially a therapy that can be translated to the clinic quite easily,” says Juan Carlos Izpisua Belmonte, lead author and a professor in Salk’s Gene Expression Laboratory. “We are excited to continue refining this promising combination therapy for human use.”
“From the very first time we tested this drug combination on just a few animals, we saw a huge improvement.” — Isabel Guillen-Guillen
Affecting 30 million adults, osteoarthritis is the most common joint disorder in the United States and its prevalence is expected to rise in the coming years due to the aging population and increasing rate of obesity. The disease is caused by gradual changes to cartilage that cushions bones and joints. During aging and repetitive stress, molecules, and genes in the cells of this articular cartilage change, eventually leading to the breakdown of the cartilage and the overgrowth of underlying bone, causing chronic pain and stiffness.
Previous research had pinpointed two molecules, alpha-KLOTHO and TGF beta receptor 2 (TGFβR2), as potential drugs to treat osteoarthritis. αKLOTHO acts on the mesh of molecules surrounding articular cartilage cells, keeping this extra-cellular matrix from degrading. TGFβR2 acts more directly on cartilage cells, stimulating their proliferation and preventing their breakdown.
While each drug alone had only moderately curbed osteoarthritis in animal models of the disease, Izpisua Belmonte and his colleagues wondered if the two drugs would act more effectively in concert.
“We thought that by mixing these two molecules that work in different ways, maybe we could make something better,” says Paloma Martinez-Redondo, a Salk postdoctoral fellow and co-first author of the new study.
The researchers treated young, otherwise healthy rats with osteoarthritis with viral particles containing the DNA instructions for making αKLOTHO and TGFβR2.
Six weeks after the treatment, rats that had received control particles had more severe osteoarthritis in their knees, with the disease progressing from stage 2 to stage 4. However, rats that had received particles containing αKLOTHO and TGFβR2 DNA showed recovery of their cartilage: the cartilage was thicker, fewer cells were dying, and actively proliferating cells were present. These animals’ disease improved from stage 2 to stage 1, a mild form of osteoarthritis, and no negative side effects were observed.
“From the very first time we tested this drug combination on just a few animals, we saw a huge improvement,” says Isabel Guillen-Guillen, also a Salk postdoctoral fellow and the paper’s co-first author. “We kept checking more animals and seeing the same encouraging results.”
“We think that this could be a viable treatment for osteoarthritis in humans.” — Pedro Guillen
Further experiments revealed 136 genes that were more active and 18 genes that were less active in the cartilage cells of treated rats compared to control rats. Among those were genes involved in inflammation and immune responses, suggesting some pathways by which the combination treatment works.
To test the applicability of the drug combination to humans, the team treated isolated human articular cartilage cells with αKLOTHO and TGFβR2. Levels of molecules involved in cell proliferation, extra-cellular matrix formation, and cartilage cell identity all increased.
“That’s not the same as showing how these drugs affect the knee joint in humans, but we think it’s a good sign that this could potentially work for patients,” says Martinez-Redondo.
The research team plans to develop the treatment further, including investigating whether soluble molecules of the αKLOTHO and TGFβR2 proteins can be taken directly, rather than administered through viral particles. They also will study whether the combination of drugs can prevent the development of osteoarthritis before symptoms develop.
“We think that this could be a viable treatment for osteoarthritis in humans,” says Pedro Guillen, director of the Clinica CEMTRO and co-corresponding author.
Man this would be great. I have it in hips and knees
No, no, no! Is has proteins in viral particles! It will kill us all!! </sarc>
I included ‘sports’ as a topic because many athletic types eventually develop osteoarthritis from the ‘wear & tear’ on their joints.................
But it has electrolytes!...................
For anyone else curious, a link to the paper...
αKLOTHO and sTGFβR2 treatment counteract the osteoarthritic phenotype developed in a rat model
Any updates since January 25, 2020? It would be a great cure for all of us arthritis sufferers.
Perhaps they can use mRNA technology to produce the two proteins where needed?
/in before expected expressions of horror at that thought
Ankles and hips for me. I have needed a cane since. I was 40.
https://freerepublic.com/focus/f-chat/3761669/posts
The paper that references speaks to a study that had a reduction of pain and movement for severe osteo arthritis patients:
In the severe OA group, average pain reduction was 47.9% at 4 weeks and 64.5% at 8 weeks. In the first 4 weeks, 40% of subjects with severe OA reduced or eliminated their analgesic (ibuprofen) use. By week 8, 75% had quit using their NSAID medication (ibuprofen). Joint rigidity disappeared in one-half of the severe OA patients in the first 4 weeks. In the remaining one-half, joint rigidity decreased significantly, an average rigidity reduction of 50%. Mobility and flexibility were significantly improved in 50% of severe OA subjects at 4 weeks and in 62.5% at 8 weeks.
The amount being given was 12 mg/day for the severe group. 20 mg/day is the Upper Tolerable Limit.
The form used was calcium fructoborate, but a common tri-boron capsule should be absorbable in a similar way.
Each pill of the following has 5.5 mg of calcium fructoborate:
Killing the pain just masks the problem. Depending on adverse reactions, sign me up for this one. Mine is Osteo and not the rheumatoid brand. I was on and off the tractors all day yesterday. Hit the bottom step, knee folded and barked my shin. Telling today.
Check out the other links posted, as well ....................
Please see post #14.
I should say, each of those pills has 5.5 mg of boron in the calcium fructoborate form.
Calcium fructoborate has only a tiny amount of the molecule as actual boron.
““We thought that by mixing these two molecules that work in different ways, maybe we could make something better,””
REALLY? You spent how much on your education to be able to figure that one out?
WOW! Its almost as ingenious as repurposing existing drugs to treat a new disease. /s
So, list you meaningful accomplishments beyond being critical of your betters
Disclaimer: Opinions posted on Free Republic are those of the individual posters and do not necessarily represent the opinion of Free Republic or its management. All materials posted herein are protected by copyright law and the exemption for fair use of copyrighted works.