By now, we all know America’s immediate COVID-19 action plan is to avoid rapid spread of the virus through good hygiene and isolation. The logic of this mitigation strategy is quite sound. As Dr. Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, has repeatedly explained, this approach will buy us time and flatten the curve of the national infection rate.
Both of these steps are needed because intensive care unit (ICU) resources are essential to managing the disease in older and sicker patients, but are inherently expensive and finite. We cannot afford to overwhelm them.
The problem with mitigation is that it is entirely defensive; it does little to make the country safe for a return to widespread social and economic activity. If and when social isolation and quarantine measures relax, coronavirus infection rates will rise in tandem.
The Imperial College has modeled the effect of imposing four interventions — social distancing of the entire population, case isolation, household quarantine, and school and university closure — then relaxing them periodically to allow daily life and economic activity to partially recover. They found, “Once interventions are relaxed … infections begin to rise, resulting in a predicted peak epidemic later in the year. The more successful a strategy is at temporary suppression, the larger the later epidemic is predicted to be in the absence of vaccination, due to lesser build-up of herd immunity.”
In other words, a mitigation strategy based on shutting down the economy is like asking society to hold its breath to keep from inhaling a toxin. It can’t keep up forever, and when it does breathe, all that gasping for air is going to undo much of the benefit we’d hoped to derive.
The alternative to mitigation is active suppression of the disease. The conventional approach for suppressing epidemics is the development of: 1) an effective vaccine and 2) drugs that could be used to reduce the severity. Despite record-time development of potential vaccines and the beginning of Phase I clinical trials, we are not likely to have a coronavirus vaccine widely available until at least mid- to late-2021. We can certainly hope effective drug therapies become available in that time, but there are certainly no guarantees.
Neither mitigation nor waiting for a vaccine is acceptable given the magnitude of the problem we are facing. Economies are like a living organism — as soon as their normal functions are shut down, they begin to die. Savings, capital, income, and taxes all evaporate. Companies begin to close, and many will not have the resources to begin again. Massive deficits will become a huge burden for future generations. Meanwhile, the regular health care system is all but shut down.
It is time to think outside the box and seriously consider a third, somewhat unconventional alternative: controlled voluntary infection (CVI).
What Is Controlled Voluntary Infection?
CVI involves allowing people at low risk for severe complications to deliberately contract COVID-19 in a socially and medically responsible way so they become immune to the disease. People who are immune cannot pass on the disease to others.
If CVI were to become widespread and successful, it could be a powerful tool for both suppressing the Wuhan coronavirus and saving the economy. It could reduce the danger of passing COVID-19 to vulnerable populations, drastically reduce the amount of social isolation needed, reopen businesses, and even help achieve the level of “herd immunity” needed to stop the spread of the disease within the population.
Herd immunity, of course, is the phenomenon whereby contagious infections can no longer spread if a large enough percentage of the population is immune to the disease, and CVI is a means to achieve it. Many over the age of 60 might remember an interesting historical precedent for CVI: chickenpox parties.
Before vaccinations for childhood diseases such as chickenpox and German measles were developed, families would hold chickenpox or German measles “parties” when one child contracted the disease. All the neighborhood children were invited to play with the infected child with the understanding that they would probably become infected as a result. The entire community would get the disease out of the way in one little local epidemic. Since many childhood diseases are far more severe if contracted as an adult, voluntary infection minimized the potential for future adverse consequences.
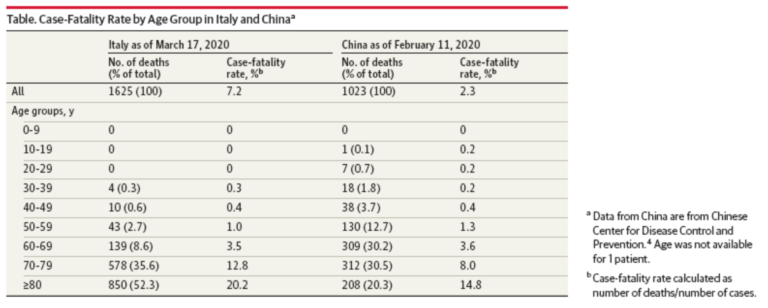
CVI for COVID-19 is based upon a unique characteristic of the Wuhan virus: Its infections are known to be clinically mild in much of the population, specifically healthy young people — even to the point of being asymptomatic. According to data collected from the National Health Institute in Italy and a recent article in the Journal of the American Medical Association, the mortality rate for the disease is 0 percent in patients 0 to 29 years old. Mortality then begins to increase with age and with underlying defects in respiratory function or certain other disease conditions. See Table 1.
Table 1: Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy.
There are exceptions, of course. According to a recently published study in the journal Pediatrics of 2,143 pediatric patients from China with confirmed or suspected cases of the Wuhan virus, one child died (0.05 percent). This is an order of magnitude lower than estimated mortality for the population as a whole.
The same study found that 10.6 percent of children under 1 year old experienced severe or critical symptoms, as did 7.3 percent of patients from 1 to 5 years old. The rate of severe illness then began to decrease with age; only about 3 percent of children 15 years old or older became seriously ill. Overall, the study found the rates of both serious disease and death in children to be far lower than the comparable rates in adults.
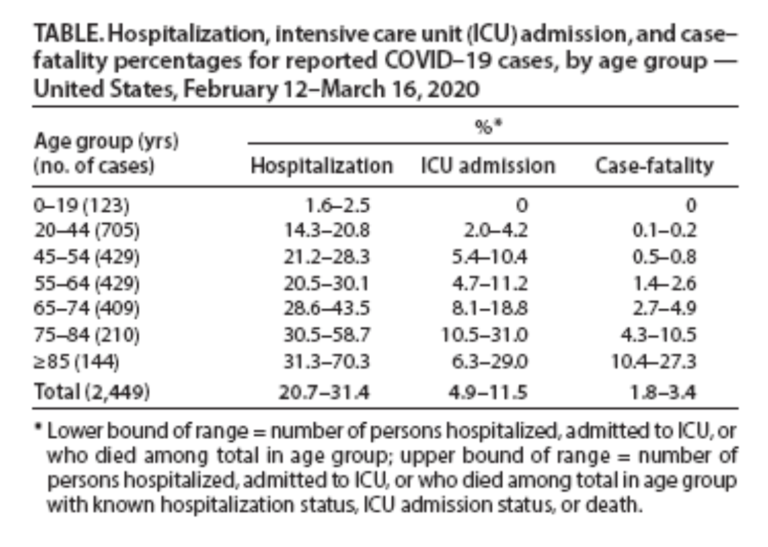
Table 2 shows the U.S. experience with pediatric and older patients through March 16, 2020. No childhood fatalities have been recorded in the United States thus far. While the incidents of hospitalization and ICU care in those aged 20 to 44 are significantly higher than those under age 19, incidents of mortality are still very low compared to those 45 and older.
Table 2: Severe Outcomes Among U.S. Patients with COVID-19 — Feb. 12 – March 16, 2020
This data shows that although there is clearly a risk associated with having younger people exposed to COVID-19, it is a risk many people might rationally decide to take. Under mitigation alone, millions of Americans will be infected with the Wuhan coronavirus one way or another. There may be considerable value in keeping careful track of who has and has not had COVID-19, and allowing people at low risk to decide whether, when, where, and how they contract the disease.
How Would CVI Work?
The basic principles are simple:
- Otherwise-healthy young people who have not yet contracted COVID-19 can enroll in the CVI program at a designated “safe infection” site.
- After being medically screened, participants are actively exposed to the mildest form of COVID-19 virus available. They are then housed under quarantine in an appropriate CVI facility. The facility could be as small as one’s home or as large as a hotel or cruise ship. (Given the recent example of spring break 2020 for college students in Florida, one could imagine CVI even becoming a social activity.)
- All participants are then regularly screened for the presence of an active COVID-19 infection and medically monitored during their illness. Patients who experience serious medical complications would be evacuated to an acute care facility. Once a patient reliably tests negative for an active infection, he or she receives a certified clean bill of immunity (CCBI) and is allowed to re-enter the community.
- A critical component of this program is widespread testing of the general population to determine exactly who has and has not already become immune to coronavirus. Those who have previously been infected and developed immunity would also be given a certified clean bill of immunity.
The potential benefits of a successful CVI program are considerable:
- For the first time, we would have a handle on exactly who in the population has been infected with the virus that causes COVID-19, and their immune status;
- Those given a CCBI could move freely, work anywhere, and be freed from social distancing. They could help treat patients, care for vulnerable populations, and keep the economy functioning when mitigation measures force others into isolation. They could also return to other normal aspects of life that those in self-imposed isolation can only dream of — freely visiting sick and elderly relatives, attending school, working in groups, and going to movies, pubs, and restaurants without fear;
- CVI could rapidly and dramatically increase overall immunity, maybe even allowing us to achieve a level of herd immunity before an effective vaccine becomes available;
- Economic activity would recover far faster and at a lower cost than would otherwise be possible — all while better protecting vulnerable people.
Math tells us how many people need to be exposed to an illness or vaccine before herd immunity develops in the community. Crunching data from the MRC Centre for Global Infectious Disease Analysis at Imperial College London implies that based on the Wuhan virus’s reproduction number, we can achieve herd immunity by immunizing somewhere between 33.3 to 71.4 percent of the population, with an averaged guess of 61.5 percent. Given the age demographic breakdown of the population, there is a good chance a safe and responsible CVI could get us close to herd immunity months before a vaccine makes 100 percent immunization possible.
Potential Limits of This Approach
The potential limitations of selective infection fall into two main categories. The first is scientific. Can we produce large numbers of reliable tests that will allow us to document individual virus immunity? The answer will be “yes.” Considerable progress has already been made toward this goal.
How persistent and reliable is the immunity that develops? Does immunity to one strain of the virus confer immunity on other known strains? Is it possible for patients who have recovered from COVID-19 to be re-infected? What is the most efficient way to safely set up and operate CVI venues? These questions should all be answerable within a relatively short period of time.
The second category is social. Does a society like ours allow people the freedom to participate in CVI programs? How do we deal with potential liability issues? Will we allow parents to make these sorts of infection decisions for both themselves and their children? Are there people who should not be allowed to participate because of age or pre-existing conditions?
If people are willing to risk deliberate infection for the sake of themselves and the greater good, should the government, and therefore taxpayers, cover any medical and hospitalization costs they may incur in the process? It is quite possible the answers to such questions might differ in various countries or even parts of a given country. Fortunately the CVI approach is amenable to implementation on any level, from communities to cities, regions, or an entire nation.
This type of controlled infection program would be unprecedented, but so is a disease with the unique clinical characteristics of COVID-19. Unfortunately, the status quo itself is hardly a safe, certain, or risk-free course of action. If the Wuhan virus pandemic is the moral and medical equivalent of war, this is exactly the sort of crash project that could save the day for millions of Americans, jobs, and future generations who will bear much of the cost of this disease.