Skip to comments.
A Viral Wonderland in the Human Gut
Science Magazine Online ^
| 14 July 2010
| Gisela Telis
Posted on 07/14/2010 7:40:34 PM PDT by Fractal Trader
Snowflakes haven't cornered the market on uniqueness. Researchers report that human guts harbor viruses as unique as the people they inhabit; the viral lineup differs even between identical twins. The discovery offers a first glimpse at the previously unknown viruses and their surprisingly friendly relationships with their hosts.
Microbiologists have known since the late 19th century that human intestines are a crowded and complicated place. Our bacterial denizens outnumber our cells, and many help break down foods and fight off pathogens. For the past decade, microbiologist Jeffrey Gordon of Washington University in St Louis has been mapping the gut's microbial landscape. His studies have linked intestinal bacteria to obesity and have shown that families tend to share their microbial makeup. But scientists hadn't yet explored whether phages—viruses that infect bacteria—were part of this shared community.
Led by graduate student Alejandro Reyes, Gordon's team analyzed fecal samples from four sets of Missouri-born female identical twins and their mothers. The researchers collected and purified the poop three times over the course of a year—to better track the microbial community's changes over time—and then sequenced the viral DNA, or viromes, the poop contained. Only 20% of the viromes matched existing databases; the rest came from previously unknown viruses. And each woman's set of viromes was distinctive, differing even from the viromes of her identical twin, the researchers report in the 15 July issue of Nature. Unlike their bacterial profiles, which overlapped by about 50% (significantly more than between strangers), identical twins had no more viruses in common than did unrelated people.
Equally surprising, Gordon says, was the communities' consistency: the viral makeup changed less than 5% over the course of the year, and the viromes of the most abundant phages changed less than 1%. Rapidly changing viromes would have signaled an "arms race" in which threatened bacteria were adapting to survive phage attacks, and the phages were adapting to avoid bacterial defenses. "The fact that the viromes didn't change," says Gordon, "suggests this is a temperate environment" in which the bacteria and their phages coexist in peace.
That may be because the viruses are actually helping the bacteria. When the viruses latch onto gut bacteria, they take some of their host's genetic material and can change it or move it to other hosts, bringing new and potentially advantageous functions to the bugs. The researchers found that many of the genes the phages carry and transfer are beneficial to the bacteria; some may help them repair cell walls, for example. In return, the bacteria, which don't die from the infections, provide an improved cellular factory to make new viruses.
The researchers don't know where the viruses come from or what causes viromes to differ so dramatically from person to person. But their data indicate that there is a huge diversity of these viruses, and that could explain why even closely related people can harbor very different populations.
Gordon says that understanding the details of the phage-bacteria relationship could help gauge the health of a patient's gut community, because the phages are sensitive to changes in their hosts. But "we still have a lot to learn about viruses" before we can expect any practical applications, says microbiologist Edward DeLong of the Massachusetts Institute of Technology in Cambridge. "This is just a first peek," he says, "but it's a remarkable one. It's the first high-resolution picture of the bacterial-viral dynamic in the human ecosystem, in a huge part of our own ecology that remains terra incognita."
TOPICS: Miscellaneous; Science; Society
KEYWORDS:
To: SunkenCiv; neverdem
FYI — I really liked this article!
To: Fractal Trader
One of the newer treatments for certain infections caused by antibiotic-resistant bacteria is to orally place fresh human faeces into the gut.
To: James C. Bennett
Isn't that what the US is already getting from vegetables imported from Mexico?
To: James C. Bennett
I’ll stick with my probiotics, thank you.
5
posted on
07/14/2010 7:51:07 PM PDT
by
goodwithagun
(My gun has killed fewer people than Ted Kennedy's car.)
To: Fractal Trader
You know it’s a serious science magazine when they use terms like “poop”.
Nevertheless, an interesting bit of research.
P.S. I would not want to be one of those grad students “purifying” poop.
6
posted on
07/14/2010 7:53:04 PM PDT
by
seowulf
("If you write a whole line of zeroes, it's still---nothing"...Kira Alexandrovna Argounova)
To: Deaf Smith
LOL! Actually one of the theories out there as to why allergies seem to be increasing is that moms of today are more paranoid about bugs and germs. The kids don’t get exposed to “dirt” like they used to and thus tolerance to some substances is not built up.
7
posted on
07/14/2010 7:54:25 PM PDT
by
BuckyKat
(Green is the new red.)
To: James C. Bennett
It’s now thought by some that the appendix serves as a reservoir for beneficial organisms in the human gut.
8
posted on
07/14/2010 7:55:08 PM PDT
by
Pelham
(treason. not just for Democrats anymore)
To: James C. Bennett
9
posted on
07/14/2010 7:56:14 PM PDT
by
justsaynomore
(The Hermanator - www.hermancain.com)
To: seowulf
P.S. I would not want to be one of those grad students “purifying” poop.Ain't that the truth?!!! My better half prior to dental school worked in a lab in Southern California that tested bodily fluids for assorted illegal substances that would subsequently used in court. He decided dentistry (usually) smelled better.
10
posted on
07/14/2010 7:57:50 PM PDT
by
BuckyKat
(Green is the new red.)
To: BuckyKat
That's from the antibiotics are in most every household product.
To: BuckyKat
That and lack of breastfeeding. I passed on so many good things to my son just by breastfeeding instead of using formula. Also, many food allergies are from parents giving kids certain foods too early. The little bodies can’t handle them and they develope an allergy. So many parents want to force their kids to eat big people food, when the best thing is to move slowly. And by the way, we never used hand sanitizer when our son was born. He is now 22 months and healthy as a horse. He has had one ear infection that we treated with probiotics. That has been his only issue.
12
posted on
07/14/2010 7:59:11 PM PDT
by
goodwithagun
(My gun has killed fewer people than Ted Kennedy's car.)
To: justsaynomore
Fecal transplants to cure Clostridium difficile infectionCategory: Antibiotic resistance • Ecology • General Epidemiology • Infectious disease • Public health • Various bacteria
Posted on: December 17, 2007 1:50 PM, by Tara C. Smith
In my field, many things that cause the average man-on-the-street to get a bit squeamish or squicked are rather commonplace. My own studies include two types of bacteria that are carried rectally in humans (and other animals), so I spend an absurd amount of time thinking about, well, shit, and the lifeforms that inhabit it and collectively make up our normal gut flora. The vast majority of these species don't harm us at all, and many are even beneficial: priming our immune system; assisting in digestion; and filling niches that could be colonized by their nastier bacterial brethren.
It's typically when there's some disturbance in these flora that bad things happen. For example, you may ingest food contaminated with a foreign bacterial strain that may transiently colonize your intestines, resulting in cramping and diarrhea. Typically these infections are self-limited and your normal flora "resets itself" after a short time, but some pathogenic bacteria have a propensity for making themselves at home in your gut. How to get rid of these nasty invaders then? Antibiotics are one option, but they also kill your regular bacteria, potentially making the problem worse (especially if the nasty invader happens to be resistant to many antibiotics). There has been a large increase in the use of probiotics--formulations designed to add beneficial bacteria to your gut. However, these have largely not been rigorously tested or regulated, so it's unsure how well they actually work.
What if, instead of re-constitituing healthy gut flora one species at a time, you could simply take the entire fecal contents from a healthy person and use it to re-colonize your own gut--in other words, undergo a fecal transplant? Yes, it's like probiotics on steroids: getting an infusion of someone else's gut flora in order to re-establish a healthy gut ecology of your own, and squeeze out some potentially harmful organisms along the way. A recent story discusses this treatment for patients suffering Clostridium difficile infections in Scotland, but it's actually not brand-new, and has already surfaced in the peer-reviewed literature. More after the jump...
First, a quick review of C. difficile, which is a spore-forming bacterium carried asymptomatically by a small percentage of us. This species has become a problem in recent years due to both the emergence of a new, more virulent strain, and apparently due to an increase in use of a certain class of antibiotics, the fluoroquinolones.
These antibiotics are termed "broad spectrum:" they kill a number of different species of bacteria in one fell swoop. This is good for the clinician, because it means they can start treatment quickly, before culture results are even back from the lab. However, it may be bad for the patient in the long term because it means that the antibiotic regimen will kill not only the bacterium causing the disease, but also will wipe out many beneficial organisms in and on the body. The result can be a disturbance in the ecology of one's normal flora, setting the stage for an invader such as C. difficile to come in and set up shop--and once it's there, it's notoriously difficult to get rid of. And once it's there and causing a symptomatic infection, it can be hell to deal with, resulting in copious and sometimes frequent diarrhea, and occasionally causes a more serious and painful condition called colitis (inflammation of the colon). Additional antibiotics can eliminate C. difficile, but they don't work for all patients, and infection can result in miserable symptoms. Thus, some have turned to the fecal transplant as a last-ditch effort to cure themselves of the infection.
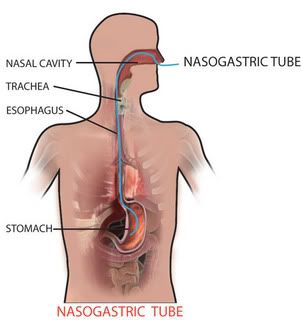
This procedure was described in a 2003 Clinical Infectious Diseases paper, documenting 19 patients who'd undergone a fecal transplant between 1994 and 2002. Donor feces are provided to the patient via a nasogastric tube as depicted in the picture to the right. 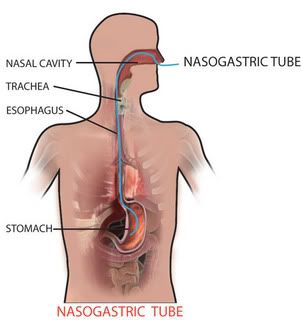 First, of course, donor stool must be procured. When possible, they used donor stool from someone the recipient would be in contact with anyway--a spouse or other household member, preferably. A fresh sample is obtained and then, um, processed. The authors describe their methods (emphasis mine):
First, of course, donor stool must be procured. When possible, they used donor stool from someone the recipient would be in contact with anyway--a spouse or other household member, preferably. A fresh sample is obtained and then, um, processed. The authors describe their methods (emphasis mine):
Select a stool specimen (preferably a soft specimen) with a weight of 30 g or a volume of 2 cm^3. Add 50-70 mL of sterile 0.9 N NaCl to the stool sample and homogenize with a household blender. Initially use the low setting until the sample breaks up; then, advance the speed gradually to the highest setting. Continue for 2-4 min until the sample is smooth. Filter the suspension using a paper coffee filter. Allow adequate time for slow filtration to come to an end. Refilter the suspension, again using a paper coffee filter. As before, allow adequate time for slow filtration.
25 mL of the suspension is then transferred to the recipient, who's already been prepared for the transplant via treatment with vancomycin (to kill off as much existing C. difficile as possible) and omeprazole (Prilosec, to decrease stomach acid production). The tube is then flushed with a salt solution and removed, and the recipient is free to go. (They were followed up either via phone or return visits to the clinic).
Was it worth it? It appeared to be a fairly successful procedure:
After the stool transplantation, 14 of the 16 surviving patients submitted a total of 20 stool samples that were tested for C. difficile toxin. Patients 3 and 11 did not submit stool samples after undergoing stool transplantation. A telephone follow‐up conversation with patient 3 and a review of the clinical record for patient 11 verified that neither patient had experienced a recurrence of diarrhea after the stool transplantation. Both patients remained free of diarrhea during the 90‐day follow‐up period.
One additional patient did develop diarrhea due to C. difficile, and was given an additional course of vancomycin (after which he was fine). Additionally, "all surviving patients reported that bowel habits returned to the functional pattern that had preceded their first episode of C. difficile colitis."
The authors acknowledge that additional research needs to be done (including clinical trials). A limitation exists in the design: one can't be certain if it was the vancomycin treatment or the fecal transplant that led to the resolution of symptoms (although the former seems unlikely, since recipients were all patients who had previously received vancomycin treatment). Additionally, there's obviously a lot of "ick" factor that needs to be overcome. There are also several logistic hurdles, such as storing and transporting feces in some cases:
"I had to collect stool samples for five days prior to our leaving Toronto, and I collected it in an ice cream container and kept it in the fridge," said [donor] Sinukoff. She had to then fly the samples to Calgary so that [Calgary physician Dr. Tom] Louie could transplant it into her sister -- a process that involved getting the sample through airport security.
"My biggest fear was that my samples were not allowed to be frozen, so I had to take them as carry-on luggage in the airplane and I was terrified that I was going to be asked to have my luggage searched," she said.
As the article quips, in the annals of medical history, this method has the potential to be one of the most effective, but also most stomach-churning.
Reference
Aas, J. et al. 2003. Recurrent Clostridium difficile Colitis: Case Series Involving 18 Patients Treated with Donor Stool Administered via a Nasogastric Tube. CID. 36:580-585. Link.
Image from http://www.disaboom.com/getfile/6e427b25-7801-4474-b794-fe8e5aab179c/NasogastricTube.aspx
To: goodwithagun
Agreed on the breastfeeding and pushing solids too early. I didn’t wean our daughter till around a year, but our son at 6 months (that kid could BITE!).
I’m not so sure about the antibiotics in household products - resistant diseases yes, allergies probably not so much.
14
posted on
07/14/2010 8:01:29 PM PDT
by
BuckyKat
(Green is the new red.)
To: BuckyKat
It seems to me to be a very credible theory.
15
posted on
07/14/2010 8:02:02 PM PDT
by
OneWingedShark
(Q: Why am I here? A: To do Justly, to love mercy, and to walk humbly with my God.)
To: OneWingedShark
Wow; the scoop on poop! Cool.
16
posted on
07/14/2010 9:35:33 PM PDT
by
QBFimi
(When gunpowder speaks, beasts listen.)
To: Fractal Trader
17
posted on
07/14/2010 10:21:15 PM PDT
by
redhead
(BP Gulf Blowout Debacle: Obama's CHERNOBYL.)
Disclaimer:
Opinions posted on Free Republic are those of the individual
posters and do not necessarily represent the opinion of Free Republic or its
management. All materials posted herein are protected by copyright law and the
exemption for fair use of copyrighted works.
FreeRepublic.com is powered by software copyright 2000-2008 John Robinson
 First, of course, donor stool must be procured. When possible, they used donor stool from someone the recipient would be in contact with anyway--a spouse or other household member, preferably. A fresh sample is obtained and then, um, processed. The authors describe their methods (emphasis mine):
First, of course, donor stool must be procured. When possible, they used donor stool from someone the recipient would be in contact with anyway--a spouse or other household member, preferably. A fresh sample is obtained and then, um, processed. The authors describe their methods (emphasis mine):