
Posted on 03/29/2020 4:18:02 AM PDT by Liz
“I am an Emergency Room MD in New Orleans, UNC class of ’98. Every one of my colleagues have now seen several hundred Covid 19 patients and this is what I think I know.
Clinical course is predictable.
2-11 days after exposure (day 5 on average) flu like symptoms start. Common are fever, headache, dry cough, myalgias (back pain), nausea without vomiting, abdominal discomfort with some diarrhea, loss of smell and taste, anorexia, fatigue.
Day 5 of symptoms- increased SOB, and bilateral viral pneumonia from direct viral damage to lung parenchyma.
Day 10- Cytokine storm leading to acute ARDS and multiorgan failure. You can literally watch it happen in a matter of hours.
81% mild symptoms, 14% severe symptoms requiring hospitalization, 5% critical.
Patient presentation is varied. Patients are coming in hypoxic (even 75%) without dyspnea. I have seen Covid patients present with encephalopathy, renal failure from dehydration, DKA. I have seen the bilateral interstitial pneumonia on the xray of the asymptomatic shoulder dislocation or on the CT’s of the (respiratory) asymptomatic polytrauma patient. Essentially if they are in my ER, they have it. Seen three positive flu swabs in 2 weeks and all three had Covid 19 as well. Somehow this ***** has told all other disease processes to get out of town.
China reported 15% cardiac involvement. I have seen covid 19 patients present with myocarditis, pericarditis, new onset CHF and new onset atrial fibrillation. I still order a troponin, but no cardiologist will treat no matter what the number in a suspected Covid 19 patient. Even our non covid 19 STEMIs at all of our facilities are getting TPA in the ED and rescue PCI at 60 minutes only if TPA fails.
Diagnostic
CXR- bilateral interstitial pneumonia (anecdotally starts most often in the RLL so bilateral on CXR is not required). The hypoxia does not correlate with the CXR findings. Their lungs do not sound bad. Keep your stethoscope in your pocket and evaluate with your eyes and pulse ox.
Labs- WBC low, Lymphocytes low, platelets lower then their normal, Procalcitonin normal in 95% CRP and Ferritin elevated most often. CPK, D-Dimer, LDH, Alk Phos/AST/ALT commonly elevated. Notice D-Dimer- I would be very careful about CT PE these patients for their hypoxia. The patients receiving IV contrast are going into renal failure and on the vent sooner.
Basically, if you have a bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that.
A ratio of absolute neutrophil count to absolute lymphocyte count greater than 3.5 may be the highest predictor of poor outcome. the UK is automatically intubating these patients for expected outcomes regardless of their clinical presentation.
An elevated Interleukin-6 (IL6) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes. Other factors that appear to be predictive of poor outcomes are thrombocytopenia and LFTs 5x upper limit of normal.
Disposition
I had never discharged multifocal pneumonia before. Now I personally do it 12-15 times a shift. 2 weeks ago we were admitting anyone who needed supplemental oxygen. Now we are discharging with oxygen if the patient is comfortable and oxygenating above 92% on nasal cannula. We have contracted with a company that sends a paramedic to their home twice daily to check on them and record a pulse ox. We know many of these patients will bounce back but if it saves a bed for a day we have accomplished something. Obviously we are fearful some won’t make it back.
We are a small community hospital. Our 22 bed ICU and now a 4 bed Endoscopy suite are all Covid 19. All of these patients are intubated except one. 75% of our floor beds have been cohorted into covid 19 wards and are full. We are averaging 4 rescue intubations a day on the floor. We now have 9 vented patients in our ER transferred down from the floor after intubation.
Luckily we are part of a larger hospital group. Our main teaching hospital repurposed space to open 50 new Covid 19 ICU beds this past Sunday so these numbers are with significant decompression. Today those 50 beds are full. They are opening 30 more by Friday. But even with the “lockdown”, our AI models are expecting a 200-400% increase in covid 19 patients by 4/4/2020.
Treatment
Worldwide 86% of covid-19 patients that go on a ventilator die. Seattle reporting 70%. Our hospital has had 5 deaths and one patient who was extubated. Extubation happens on day 10 per the Chinese and day 11 per Seattle.
Plaquenil (hydroxy-chloroquine) which has weak ACE2 blockade doesn’t appear to be a savior of any kind in our patient population. Theoretically, it may have some prophylactic properties but so far it is difficult to see the benefit to our hospitalized patients, but we are using it and the studies will tell.
With Plaquenil’s potential QT prolongation and liver toxic effects (both particularly problematic in covid 19 patients), I am not longer selectively prescribing this medication as I stated on a previous post.
We are also using Azithromycin.
Do not give these patient’s standard sepsis fluid resuscitation. Be very judicious with the fluids as it hastens their respiratory decompensation. Outside the DKA and renal failure dehydration, leave them dry.
Proning vented patients significantly helps oxygenation. Even self proning the ones on nasal cannula helps.
Vent settings- Usual ARDS stuff, low volume, permissive hypercapnia, etc. Except for Peep of 5 will not do. Start at 14 and you may go up to 25 if needed.
Do not use Bipap- it does not work well and is a significant exposure risk with high levels of aerosolized virus to you and your staff. Even after a cough or sneeze this virus can aerosolize up to 3 hours.
The same goes for nebulizer treatments. Use MDI. you can give 8-10 puffs at one time of an albuterol MDI. Use only if wheezing which isn’t often with covid 19. If you have to give a nebulizer must be in a negative pressure room; and if you can, instruct the patient on how to start it after you leave the room.
Do not use steroids, it makes this worse. Push out to your urgent cares to stop their usual practice of steroid shots for their URI/bronchitis. We are currently out of Versed, Fentanyl, and intermittently Propofol. Get the dosing of Precedex and Nimbex back in your heads.
One of my colleagues who is a 31 yo old female who graduated residency last may with no health problems and normal BMI is out with the symptoms and an SaO2 of 92%. She will be the first of many.
I PPE best I have. I do wear a MaxAir PAPR the entire shift. I do not take it off to eat or drink during the shift. I undress in the garage and go straight to the shower. My wife and kids fled to her parents outside Hattiesburg.
The stress and exposure at work coupled with the isolation at home is trying. But everyone is going through something right now. Everyone is scared; patients and employees.
But we are the leaders of that emergency room. Be nice to your nurses and staff. Show by example how to tackle this crisis head on. Good luck to us all."
I love seeing the fearbros out in the morning.
“Dudes- we’re all gonna die because there’s no cure and no treatment unless you all do what I say. Don’t get it.”
Yeah - real helpful, fearbros.
Exactly. Actual docs in the trenches are trying to share what they have learned in real time.
If they wait for peer-reviewed journals, weeks will be lost and many more patients will die.
Think Drudge.....but more conservative.
The average age of those dying is......?

If it was really written by an ER doc
This simply is not true.
1. Peep of +10 to start no one in my treatments have required PEEP of +15. It would be malpractice to dial in a PEEP of +25. He loses all credibility there. If you were to use a High PEEP he would if legit have used APRV ventilations
2. Prolonged qT is not a wide ranging side effect. He is trying to throw some shade at a testament protocol
3. The combination of Plaquenil and azithromycin in almost all studies is showing significant benefit. See French study of yesterday. Most lall
Hospitals in America are using thise combo. For my critical care unit PUI are place on this combination. For those who test (+) we are seeing either failure to progress to vent or coming off the vent more quickly.
4. He is incorrect in the anectdoatal RLL statement. Any basic medical students knows this is an aspiration finding. There was an article a few days ago which this post place rises that said something about this. Most radiologists and clinicians will tell you if there is a favored love its the bilateral upper lines
5. He fails to mention prone ventilation. Anyone who is serious would probe a patient well before a PEEP of +25
I am so sorry to poly out this is an unsourced internet plate risk that has spread from several sources and is not consistent with any clinical expertise. The above five errors are glaring. People want to believe what they want to believe I guess. But this is incorrect. There is worldwide data softening bother the scope and severity of this virus. We are getting a far better handle on who it affects and why. We have valid and decent treatment options that will continue to be used. It’s easy to amass a bunch of internet things and work it into a well written though totally incorrect document such as this
If you want to be scared then be scared but please stop spreading incorrect clinical information. The real ER docs deserve much better than this
I think the narrative posted here is floating around under “ER Doc in Nawlins”, “ER Doc in Chicago,” “ER Doc in NYC,” but all the rest is verbatim the same.
Smells like an urban rumor.

Do you think the national death numbers week over week posted at 37 were faked?
All part of a grand hoax?
My local rescue squad tells me there is no huge demand for their services this year bur just the normal flu season at the old folks homes....
Of course....sharing medical experiences is invaluable....but its not the be-all and end-all of virus treatments.
For the past several years, I have been plotting and comparing week to week influenza mortality data gathered by the National Center for Health Statistics (NCHS) mortality surveillance system. The number of coded flu deaths per year is only a part of the estimated flu deaths each week. I added US coronavirus deaths by week to the plot and got this:
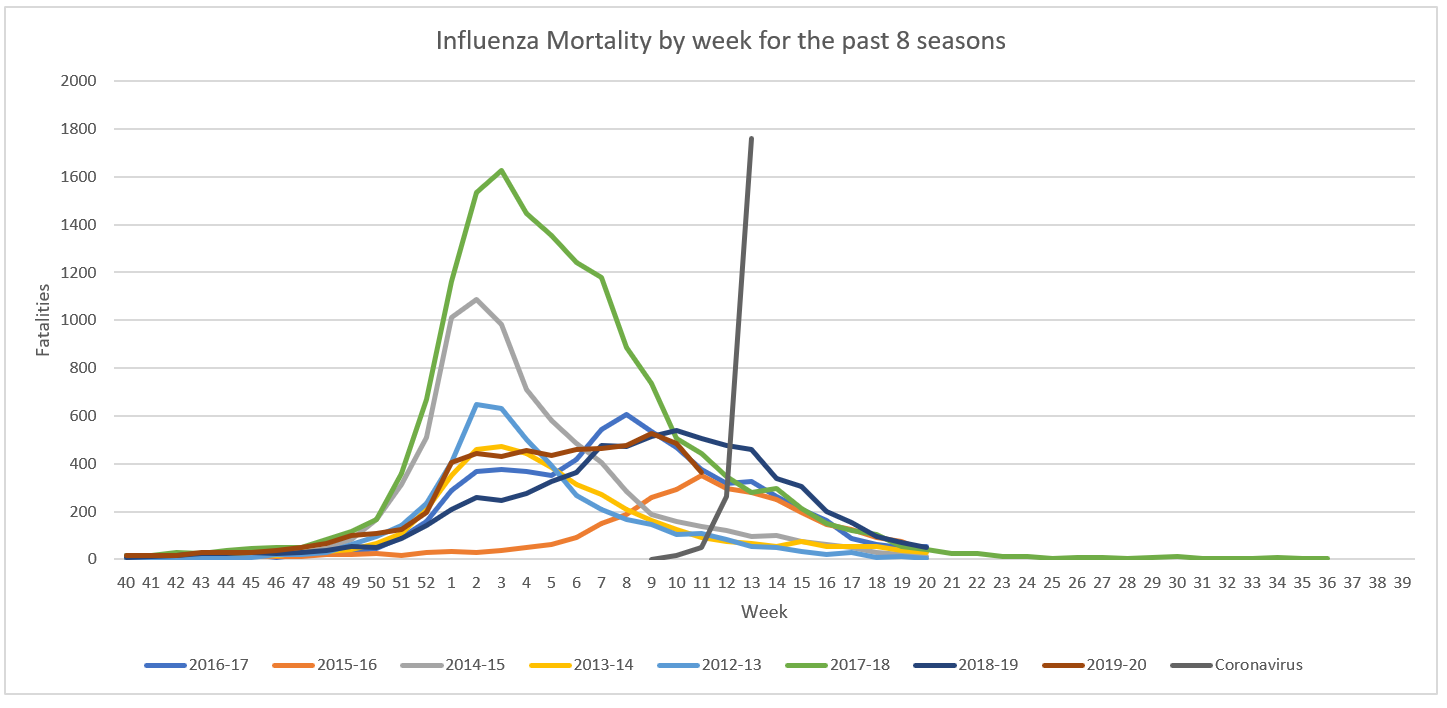
I know it's not apples to apples, the estimated number of flu deaths is about 6 times higher than the numbers recorded by the NCHS, but there is every reason to believe that the actual number of coronavirus fatalities is also larger than the subset that gets confirmed. There has only been 4 weeks of data. Where is this going to end up? https://flutrackers.com/forum/forum/-2019-ncov-new-coronavirus/united-states-2019-ncov/842586-comparing-flu-and-covid-19-deaths#post842586
Again, FEARBRO TROLL,
How come your scary chart here shows 1800 deaths but your scary chart above shows 1250?
BTW this article has been in FR for at least the last 4-5 days. It didn't just time out today.
No. Dead is dead. I think some of the cause may be misattributed, but that's to be expected.
-- All part of a grand hoax? --
I'm under "lockdown." No hoax. How is the government acting unwisely? Too early to do a post mortem on that question.
And if it didn't, this is proof that it's all a hoax.
(Some of us paid attention in math and science classes.)

I wonder whether people who have had the full regiment of pneomonia shots fare better than those who have not.
Yes travis HOAXING BY DEMOCRATS on steroids.
All numbers cherry picked and manipulated.
Amplified by blue state cadres of liberal democrats.
I’m just posting hard numbers.
Too many still think it’s all a hoax or a joke.
I’m leaving politics to others.
Disclaimer: Opinions posted on Free Republic are those of the individual posters and do not necessarily represent the opinion of Free Republic or its management. All materials posted herein are protected by copyright law and the exemption for fair use of copyrighted works.